Keratoconus
If you’re experiencing blurred vision, increased light sensitivity, or difficulty seeing well despite wearing glasses or contacts, you may be dealing with keratoconus. At Kovach Eye Institute, our board-certified ophthalmologists provide comprehensive keratoconus treatment throughout Chicago and the Chicagoland area, specializing in advanced surgical solutions including corneal cross-linking and corneal transplant procedures.
What is Keratoconus?
Keratoconus is a progressive eye condition where the cornea—the clear, dome-shaped front surface of your eye—gradually thins and bulges outward into a cone-like shape. This irregular corneal shape prevents light from focusing properly on the retina, resulting in distorted and blurred vision.
According to Johns Hopkins Medicine, keratoconus affects approximately 1 in 2,000 people, typically beginning during the teenage years or early twenties.
Trusted Source
Keratoconus
Johns Hopkins Medicine
Go to Source
1
The condition usually affects both eyes, though one eye may be more severely affected than the other.
What Are the Symptoms of Keratoconus?
Keratoconus symptoms typically develop gradually. Signs of keratoconus may include:
- Blurred or distorted vision
- Increased sensitivity to light (photophobia)
- Glare and halos around lights
- Frequent changes in eyeglass or contact lens prescriptions
- Sudden worsening or clouding of vision
- Eye strain and headaches
- Difficulty driving at night
Trusted Source Keratoconus National Library of Medicine Go to Source 2
In the early stages, keratoconus may be mistaken for astigmatism. However, as the condition progresses, standard glasses and soft contact lenses become less effective at correcting vision problems.

Causes of Keratoconus
The exact cause of keratoconus is not fully understood, but experts believe it develops from a combination of genetic predisposition and environmental influences that weaken the cornea over time. While anyone can develop keratoconus, certain factors may increase the likelihood:
- Family history: Around 1 in 10 people with keratoconus has a close relative with the condition.
Trusted Source title Mayo Clinic Go to Source 3
- Eye rubbing: Frequent or vigorous rubbing can place stress on the cornea and may accelerate progression.
- Chronic eye irritation: Ongoing issues such as dry eye, allergies, or poorly fitted contact lenses can contribute to corneal weakening.
- Medical conditions: Keratoconus has been associated with systemic conditions like asthma, Down syndrome, and retinitis pigmentosa.
Because keratoconus often begins in the teenage years or early adulthood, regular eye exams are key to detecting changes early and protecting long-term vision.
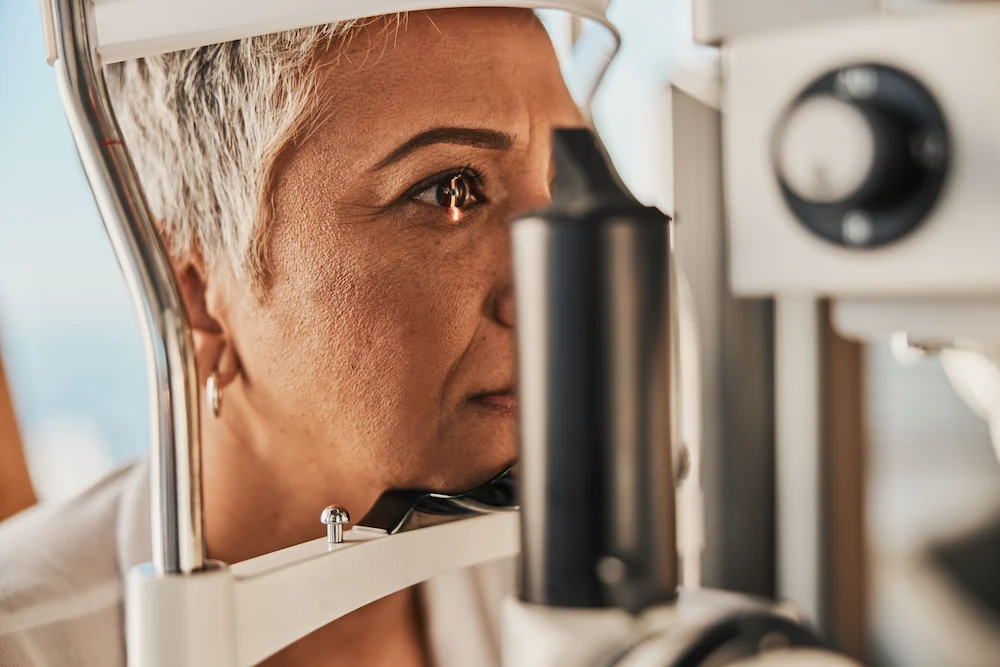
How is Keratoconus Diagnosed?
Accurate diagnosis is essential for effective keratoconus treatment. Our diagnostic process is based on a thorough eye exam that includes:
- Corneal Topography: Creates detailed maps of the corneal surface to detect irregular curvature
- Pachymetry: Measures corneal thickness to assess disease severity
- Slit-lamp Examination: Allows detailed visualization of corneal structure
- Optical Coherence Tomography (OCT): Provides cross-sectional images of corneal layers
Advanced Treatment Options for Keratoconus
At Kovach Eye Institute, we offer advanced treatment options that are designed to slow the progression of keratoconus and preserve your vision. Every treatment plan is personalized based on the stage of the disease, the condition of your cornea, and your individual visual needs.
Corneal Cross-Linking (CXL)
Corneal collagen cross-linking (CXL) is the only FDA-approved procedure proven to stop or slow the progression of keratoconus. This minimally invasive treatment works by strengthening the corneal tissue and the collagen fibers within it, helping it resist further bulging and thinning.
During the procedure:
- Riboflavin (vitamin B2) eye drops are applied to the surface of the cornea
- The cornea is then exposed to a controlled dose of ultraviolet (UV) light
- The interaction between riboflavin and UV light (ultraviolet light) creates new bonds between collagen fibers, reinforcing the cornea’s structure
While CXL does not reverse keratoconus or restore lost vision, it is highly effective in stabilizing the condition. Research has shown that CXL can reduce disease progression by up to 90% in appropriate candidates, helping patients preserve their vision and delay or avoid the need for a corneal transplant in the future.
Trusted Source
Effect of corneal cross-linking versus standard care on keratoconus progression in young patients: The KERALINK randomized controlled trial
Larkin DFP, Chowdhury K, Burr JM, Raynor M, Edwards M, Tuft SJ, et al; on behalf of the Keralink Trial Study Group
Go to Source
4
Corneal Transplant Surgery
For patients with advanced keratoconus—especially those whose vision can no longer be managed with specialty contact lenses or cross-linking—a corneal transplant may be the best option. Kovach Eye Institute offers both full-thickness and partial-thickness transplant techniques, ensuring that each patient receives the most suitable approach for their unique case.
Types of Corneal Transplants include:
- Penetrating Keratoplasty (PK or PKP): The entire damaged cornea is replaced with healthy donor tissue. This is the most common transplant type for advanced keratoconus.
- Deep Anterior Lamellar Keratoplasty (DALK): Only the outer and middle layers of the cornea are replaced, leaving the patient’s own healthy inner layers intact. DALK often results in faster recovery and a lower risk of graft rejection.
Corneal transplants are typically performed on an outpatient basis under local anesthesia. Following surgery, patients use prescription eye drops to reduce inflammation and prevent infection. With proper post-operative care and monitoring, success rates for corneal transplants in keratoconus patients exceed 90%.
Trusted Source
Frequently Asked Questions about Eye Banking, Corneas, and Transplantation
Eye Bank Association of America
Go to Source
5
Frequently Asked Questions
Kovach Eye Institute offers comprehensive keratoconus treatment at multiple locations throughout the Chicago area, including Elmhurst, Lincolnwood, Naperville, and South Barrington. Our board-certified ophthalmologists specialize in advanced surgical treatments including corneal cross-linking and transplant procedures.
Ideal candidates for corneal cross-linking typically have progressive keratoconus with adequate corneal thickness (usually >400 microns). A comprehensive evaluation including corneal topography and pachymetry will determine your candidacy for this procedure.
If keratoconus continues to progress despite cross-linking treatment, corneal transplant surgery may be recommended. Our surgeons have extensive experience with both traditional and advanced transplant techniques, with success rates exceeding 90%.
Treatment costs vary depending on the procedure and insurance coverage. Most insurance plans cover medically necessary keratoconus treatments. We provide detailed cost estimates during your consultation and offer financing options for out-of-pocket expenses.

Get started on your path to better vision with our Cornea Specialists.
We have four convenient locations in Illinois: Elmhurst, Naperville, South Barrington, and Lincolnwood. Schedule an appointment today by calling us at 630-318-4925 or request an appointment online.
1 Johns Hopkins Medicine. Keratoconus. Available: https://www.hopkinsmedicine.org/health/conditions-and-diseases/keratoconus. Accessed August 19, 2025.
2 National Library of Medicine. Keratoconus. Available: https://medlineplus.gov/ency/article/001013.htm. Accessed August 19, 2025.
3 Mayo Clinic. Keratoconus. Available: https://www.mayoclinic.org/diseases-conditions/keratoconus/symptoms-causes/syc-20351352. Accessed August 20, 2025.
4 Larkin DFP, Chowdhury K, Burr JM, Raynor M, Edwards M, Tuft SJ, et al; on behalf of the Keralink Trial Study Group. Effect of corneal cross-linking versus standard care on keratoconus progression in young patients: The KERALINK randomized controlled trial. Ophthalmology. 2021;128(11):1516–1526. doi:10.1016/j.ophtha.2021.04.019. Available: https://www.aaojournal.org/article/S0161-6420(21)00297-9/fulltext. Accessed August 19, 2025.
5Eye Bank Association of America. Frequently Asked Questions about Eye Banking, Corneas, and Transplantation. Available: https://restoresight.org/cornea-donation/faqs/. Accessed August 19, 2025.
The doctors at Kovach Eye Institute have either authored or reviewed and approved this content.
Page Updated: