Diabetic Retinopathy
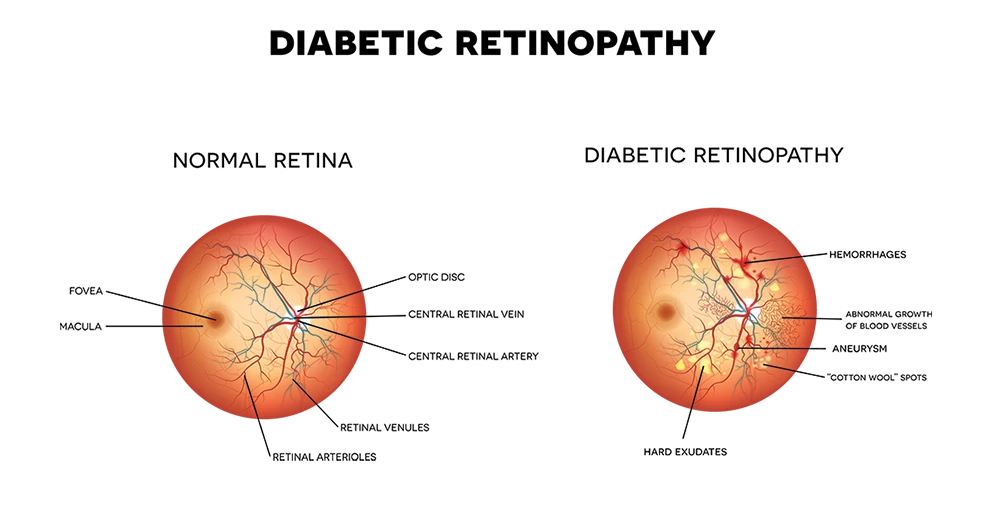
Diabetic retinopathy is a complication of diabetes that is caused by the blood vessels of the eye. The retina is a nerve layer at the back of the eye that senses light and helps to send images to your brain. When blood vessels in the retina are damaged, they may leak fluid or blood, and grow fragile, brush-like branches and scar tissue. This can blur or distort the images that the retina sends to the brain, and may lead to blindness if left untreated. Diabetic retinopathy is the leading cause of new blindness among adults in the United States. People with untreated diabetes are said to be 25 times more at risk for blindness than the general population.
If you have diabetes, it’s important to know that with today’s improved methods of diagnosis and treatment, only a small percentage of people who develop retinopathy have serious vision problems.
Types of diabetic retinopathy
Background retinopathy is an early stage of diabetic retinopathy. In this stage, tiny blood vessels within the retina become damaged and leak blood or fluid. Leaking fluid causes the retina to swell or form exudates. Sometimes the leaking fluid collects in the macula, the part of the retina that lets us see fine details like letters or numbers. This problem is called macula edema. Reading and close work may become more difficult because of this condition.
Proliferative retinopathy describes the changes that occur when new, abnormal blood vessels begin growing on the surface of the retina.
The abnormal growth is called neovascularization. These new blood vessels have weaker walls and may break and bleed into the vitreous cavity. The vitreous is the clear, Jelly-like substance that fills the center of the eye. Leaking blood can cloud the vitreous and partially block the light passing through the pupil towards the retina, causing blurred and distorted images.
The neovascularization can also lead to problems such as severe glaucoma and retinal detachments, which may lead to blindness.
Proliferative diabetic retinopathy is the most serious form of diabetic retinal disease. It affects up to 20 percent of diabetics and can cause severe loss of sight including blindness.
What are the symptoms of diabetic retinopathy?
Initially, there are usually no symptoms of background retinopathy, although gradual blurring of vision may occur if macular edema is present. As diabetic retinopathy progresses and bleeding occurs, your sight may become hazy, spotty or even disappear altogether. While there is no pain, proliferative retinopathy is a severe form of the disease and requires immediate medical attention. Pregnancy and high blood pressure may aggravate diabetic retinopathy.
Diabetic retinopathy treatments:
- Laser Treatments – These laser treatments are also known as photocoagulation and is used to stop or slow the leakage of blood and fluid in the eye.
- Intraocular Corticosteroids – Many studies have been conducted recently with these types of injections. They may reduce retinal swelling and improve visual acuity in patients with diabetic macular edema.
- Vitrectomy – A vitrectomy may be performed to clear blood and debris from the eye, to remove scar tissue, or to alleviate traction on the retina.
Learning to live with diabetes and diabetic retinopathy
If you are a diabetic patient you have most likely had some kind of discussion with your primary care doctor regarding diet. The nutrition of the food you eat becomes critical for maintaining proper blood sugar levels. Please refer to this list below for diabetic nutrition tips:
- Reduce saturated fats and avoid trans fats
- Include vegetables in your diet
- Increase fiber intake
- Reduce caffeine and refined sugar

Get started on your path to a better healthy vision with our Retina Specialist. We have four convenient locations in Illinois: Elmhurst, Naperville, South Barrington, and Lincolnwood. Schedule an appointment online or by calling us at 630-517-9312 .
The doctors at Kovach Eye Institute have either authored or reviewed and approved this content.
Page Updated: